Just Diagnosed
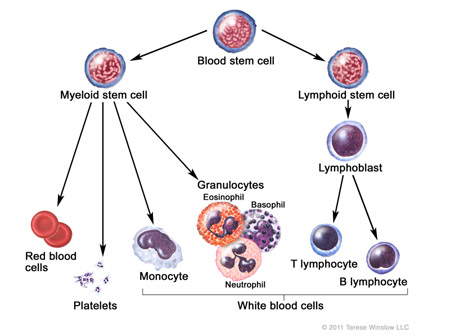
Acute myeloid leukemia (AML) is a cancer of the blood that starts in the bone marrow and spreads to the bloodstream. It is more common in adults, but each year approximately 500 new cases of AML are diagnosed in children in the United States.
Symptoms of AML
Leukemia cells "crowd out" the normal blood cells. It is the decrease in normal cells that produces the symptoms of leukemia, which may include:- Fatigue and being pale results from a decreased number of red blood cells, known as anemia.
- Fever due to the disease itself or from infection because there are a decreased number of healthy white blood cells, known as neutropenia.
- Bruising or bleeding from decreased platelets, known as thrombocytopenia.
- Bone pain that is sometimes associated with swelling of the joints.
Diagnosing Acute Myeloid Leukemia Diagnosed
A number of tests are performed to evaluate a child suspected of having leukemia. The initial test will be a blood test called a complete blood count (CBC). Your pediatrician or family doctor may order blood tests before referring your child to a specialist. Those tests are often repeated by the oncologist.
Although leukemia cells may be found in the blood, most commonly the diagnosis and classification of leukemia is confirmed by looking at a sample of bone marrow under the microscope. This sample is obtained by performing a bone marrow aspirate. A bone marrow aspirate will provide information regarding the subtype of AML.
An additional test that may be performed along with the bone marrow aspirate is the bone marrow biopsy. A bone marrow biopsy may help in making a diagnosis when there are too few cells in the aspirate sample.
A spinal tap is usually performed to look for leukemia in the central nervous system.
Following these tests, your doctor will ask the laboratory to perform cytogenetic tests (tests that check the leukemia’s chromosomes for mistakes, also called mutations). Not all chromosome mutations are easily found and sometimes they can only be seen using powerful laboratory techniques called molecular analysis (tests that look inside the chromosomes for extremely tiny mistakes). These tiny molecular mutations of the chromosomes may have a powerful impact upon the ability to be cured and have recently become the target of new medical treatments of leukemia. Based upon the chromosomal findings, your doctor can diagnosis the subtype of AML and can make an initial prognosis (prediction) for the chances of relapse and long-term cure.
Types of AML
AML can be divided into different subtypes which help your doctor determine both the general prognosis for cure as well as the best type of treatment.
About 75-80% of children with AML will have leukemia blast cells that contain poorly formed chromosomes compared to the rest of their body’s chromosomes. These abnormal chromosomes were first formed when one of the normal myeloid cells divided to make a copy of itself (which they do millions of times a day in each of us). The new copy with the abnormal chromosomes was the very first leukemia cell. This is sometimes called an acquired mutation, meaning the person was not born with it. Many types of abnormalities in the chromosomes can result in a normal myeloid cell becoming a leukemia cell.
There are some types of abnormal chromosome structure that provide information regarding response to therapy. The abnormal chromosomes that cause AML which can more easily be cured are call “low risk” mutations, and those that cause subtypes of AML that are hard to cure are called “high risk” mutations. Risk in this case means both risk for relapse and risk for treatment failure.
Research is continually working to discover all of the mutations that result in AML and other cancers. Some of the research on these mutations has led to the discovery of new ways to treat cancer. Research has determined that these mutations often create either an abnormal protein within our cells that cause them to multiply out of control, or these mutations create copies of normal proteins that are missing the function that stops cells from multiplying.
Consider it similar to a copy machine with either the “start” button stuck on copy, or the “stop” button broken and unable to stop the machine from making millions of copies. You can imagine how that would quickly fill up a room preventing it from be able to be used. The same thing happens in a person’s organs when cancer cells multiply out of control. The new treatment approaches to cancer take advantage of this new knowledge and attempt to either block the abnormal protein from causing uncontrolled copying or replace the missing “stop” protein in order to prevent the copying.
Unfortunately, each of the hundreds of types of mutations has a different protein it produces or fails to produce. Therefore, for each type of mutation (or subtype of AML), a different medication may need to be discovered and created. Researchers hope that some of these mutations can be “grouped” together and be treated with similar, new medicines so patients don’t have to wait for a new medicine to be created for every subtype.
Risk Classification
Currently, among the many types of mutations that cause AML, there are only a few that are known to impact risk of treatment failure. These are grouped into low or high risk for treatment failure below. This grouping of risk types of AML comes from the Children’s Oncology Group’s research into AML therapy and is based upon the subtypes of AML defined by the World Health Organization’s WHO 2008 Myeloid Classification publication. The names for these AML subtypes are either based upon the chromosome number on which the mutation can be found by cytogenetic testing or upon the specific gene mutations within the chromosomes found by molecular analysis.
Low-Risk AML Mutations
Cytogenetically Diagnosed Molecularly DiagnosedInversion 16 AML CEBPα AML
8;21 AML NPM (nucleophosmin) AML
High-Risk AML Mutations
Cytogenetically Diagnosed Molecularly DiagnosedMonotony 7 AML FLT3 high allelic ratio AML
Abnormal Chromosome 5q AML
These categories of AML are constantly changing with new subtypes of AML being added or old subtypes being removed from these risk groups as research progresses and new therapies occur. The subtypes of AML not included in the above categories are often called intermediate (or average) risk AML.
Finally, how one responds to treatment AML is also important in determining treatment failure risk and future therapy options for a patient. For AML patients who have remaining (also called residual) leukemia cells visible within the bone marrow after one course of chemotherapy, the chance of long-term treatment failure is high.
So, a doctor will combine the findings of the cytogenetic and molecular tests with the bone marrow tests after the first course of chemotherapy to determine whether the child’s AML is a “high risk” or “low risk” subtype. High-risk AML likely needs more therapy or new types of treatment for a better chance at cure. Low-risk AML suggests that it has a good chance of being cured using current, conventional forms of therapy.
Determining the Extent of Disease
Since AML is a cancer of the blood, it is widespread at diagnosis and does not need to be "staged" in the way solid tumors are. There are no X rays that determine the extent of the disease. However, leukemia cells can also be present in the spinal fluid, which is known as Central Nervous System (CNS) disease. A special test known as a spinal tap or lumbar puncture will be performed to obtain fluid for examination.
In addition to being present in the bone marrow and blood, leukemia can spread to areas that are part of the blood system, causing enlargement of the organs. It can affect:- Lymph nodes
- Liver
- Spleen
- Testes
- Skin
- Gums
Involvement of other organs other than the CNS usually has no bearing on the type of treatment given.
Last updated September, 2011
About Acute Myeloid Leukemia
In Treatment for Acute Myeloid Leukemia
After Treatment for Acute Myeloid Leukemia